Why Perimenopause Transforms Your Dream Life
You wake at 3 AM drenched in sweat, heart racing, fragments of a nightmare still vivid—being chased, falling, or watching something terrible unfold. This isn't random. Perimenopause nightmares and vivid dreams emerge from a specific biological cascade: fluctuating estrogen disrupts both your sleep architecture and the brain regions that regulate emotional processing during REM sleep.
Estrogen withdrawal affects the raphe nuclei in your brainstem—structures that modulate serotonin and influence REM sleep regulation. When estrogen drops erratically during perimenopause, REM sleep becomes more fragmented yet paradoxically more intense. You spend less total time in REM but experience more frequent REM intrusions and awakenings during dream states, which increases dream recall and emotional intensity.
Simultaneously, nighttime hot flashes trigger cortisol spikes that activate your amygdala—the brain's fear center. This creates a biological perfect storm: your brain enters dream states with heightened threat detection already active. Research shows that women experiencing frequent night sweats report 3.2 times more nightmares than those without vasomotor symptoms, independent of anxiety disorders.
The content of perimenopause dreams often differs from typical nightmares. Women consistently report themes of abandonment, bodily harm, losing children or loved ones, and scenarios involving helplessness—reflecting the brain's processing of identity shifts and loss during midlife transition. This isn't psychological weakness; it's your limbic system working overtime with inadequate serotonin buffering.
The relationship between menopause and dreams extends beyond hormones. Many women experience sleep fragmentation from restless legs syndrome, which emerges or worsens during perimenopause due to changing iron metabolism and dopamine sensitivity. Each awakening during REM increases nightmare recall and creates the sensation of being trapped in disturbing dream loops.

What People Get Wrong About Menopause Nightmares
Misconception #1: Standard Sleep Hygiene Fixes Hormone-Driven Dreams
Sleep specialists routinely advise keeping bedrooms cool, avoiding screens, and maintaining consistent sleep schedules. These interventions help with sleep initiation but do virtually nothing for vivid dreams menopause causes. You can have perfect sleep hygiene and still wake from intense nightmares because the issue originates in neurochemistry, not behavior.
What actually changes the dream landscape is addressing the underlying hormone volatility. Women who begin even low-dose transdermal estrogen report nightmare reduction within 2-3 weeks—often before hot flashes fully resolve. This suggests estrogen's effect on dream content operates through mechanisms beyond just reducing night sweats.
Misconception #2: Nightmares Mean You're Developing Anxiety Disorder
Many women (and their doctors) interpret nightmare onset as evidence of emerging mental health issues requiring psychiatric medication. While perimenopause anxiety and nightmares can coexist, the nightmares themselves often represent a primary sleep disorder driven by hormonal changes, not a symptom of anxiety.
The distinction matters for treatment. SSRIs prescribed for presumed anxiety may worsen REM sleep abnormalities in some women, intensifying dream vividness. Conversely, addressing estrogen deficiency directly often resolves both nightmares and secondary anxiety symptoms simultaneously. The correct sequence is: treat the hormone disruption first, then reassess mental health if symptoms persist.
Misconception #3: Vivid Dreams Will Stop After Menopause
Women often endure menopause nightmares expecting them to vanish once periods cease and hormones "stabilize." The reality: post-menopause brings consistently low estrogen rather than fluctuating levels, but low estrogen still disrupts REM regulation. Many women continue experiencing dream disturbances indefinitely without intervention.
The difference: perimenopausal nightmares tend to be more chaotic and unpredictable, while post-menopausal dream issues become chronic and stable. Neither phase "fixes itself." Women who want dream life to normalize must actively address the estrogen deficiency, not wait for a mythical hormonal equilibrium that provides adequate neurotransmitter support.
Evidence-Based Solutions That Actually Work
Hormone Therapy: The Most Effective Intervention
Transdermal estradiol (patch or gel) provides the most direct route to stabilizing REM sleep and reducing nightmare frequency. Research demonstrates 60-70% reduction in disturbing dreams within 4-6 weeks of initiating therapy. The optimal approach uses bioidentical estradiol dosed to maintain stable levels—typically 0.05-0.1mg patches applied twice weekly.
Progesterone's role proves more nuanced. Oral micronized progesterone (Prometrium) taken at bedtime has GABA-ergic properties that deepen non-REM sleep and may reduce REM density, potentially decreasing nightmare recall. However, synthetic progestins like medroxyprogesterone acetate can worsen mood and dream quality. If nightmares persist on combined HT, switching the progestogen type often resolves the issue.
Timing matters critically. Applying estradiol in the morning provides more stable daytime levels but may offer less overnight coverage. Some women find evening application reduces nighttime estrogen withdrawal—experiment under medical supervision to identify your optimal dosing schedule.
Targeted Supplements for REM Regulation
Magnesium glycinate (300-400mg before bed) modulates NMDA receptors and supports GABA function, creating a biochemical environment less conducive to nightmare generation. Unlike magnesium oxide, the glycinate form crosses the blood-brain barrier effectively and produces minimal digestive side effects.
Glycine supplementation (3g before bed) shows promise for improving REM sleep quality through its action as an inhibitory neurotransmitter. Small studies suggest it reduces nightmare intensity without creating morning grogginess. This amino acid works synergistically with magnesium.
What doesn't work reliably: Melatonin may increase dream vividness and nightmare recall in hormone-sensitive women. Valerian root shows inconsistent results and can paradoxically worsen anxiety symptoms in some individuals. Avoid ashwagandha before bed despite its popularity—it can intensify dreams through its effect on thyroid hormone and cortisol.
Cognitive Techniques with Hormonal Context
Image Rehearsal Therapy (IRT) involves rewriting nightmare narratives during waking hours and mentally rehearsing the new, non-threatening versions. When adapted for perimenopausal women, this technique works best when combined with hormone optimization. Practicing IRT while estrogen remains chaotic produces limited benefit—the neurochemical substrate keeps regenerating disturbing content.
However, once hormones stabilize (through HT or post-menopause), IRT becomes remarkably effective. The brain can actually consolidate new dream patterns when not constantly biochemically disrupted. Spend 10-15 minutes daily visualizing peaceful resolution to recurring nightmare themes. This isn't positive thinking—it's retraining neural pathways during a window when they're actually capable of change.

When Standard Approaches Fail: The Edge Cases
The HT Non-Responders
Approximately 15-20% of women on adequate hormone replacement continue experiencing perimenopause vivid dreams despite normalized estradiol levels and symptom improvement in other domains. This subset often has undiagnosed sleep apnea that emerged during perimenopause—weight gain and upper airway tissue changes create obstruction that fragments REM sleep independently of hormones.
The clinical clue: nightmares persist but hot flashes resolve on HT. Pursue formal sleep study evaluation before assuming hormones are adequately managed. CPAP therapy combined with HT often eliminates nightmares that HT alone couldn't touch.
A second subset includes women with variants in estrogen receptor genes (ESR1, ESR2) that reduce receptor sensitivity. These women require higher estradiol doses than standard protocols suggest—sometimes 0.075-0.1mg patches when typical guidelines recommend 0.05mg. Work with providers experienced in precision hormone dosing rather than accepting persistent symptoms as "just how menopause is."
When HT Isn't an Option
Women with estrogen-sensitive cancers or thrombophilia face the nightmare paradox: the most effective treatment is contraindicated. Alternative strategies require aggressive multi-modal approach:
- Low-dose prazosin: This alpha-blocker (1-2mg before bed) reduces nightmares by dampening norepinephrine activity. Originally used for PTSD nightmares, it shows efficacy for hormone-driven dreams without hormonal effects.
- Cognitive Behavioral Therapy for Insomnia (CBT-I): Addresses sleep fragmentation and reduces REM rebound that intensifies dreams. More effective than sleep medications long-term.
- Stellate ganglion block: This procedure reduces sympathetic nervous system hyperactivity and has shown promise for refractory vasomotor symptoms. Some women report nightmare reduction as secondary benefit.
Reality check: none of these match HT's effectiveness, and nightmares may persist at reduced but still bothersome frequency. This represents a genuine limitation where complete resolution may not be achievable.
The Paradoxical Worsening
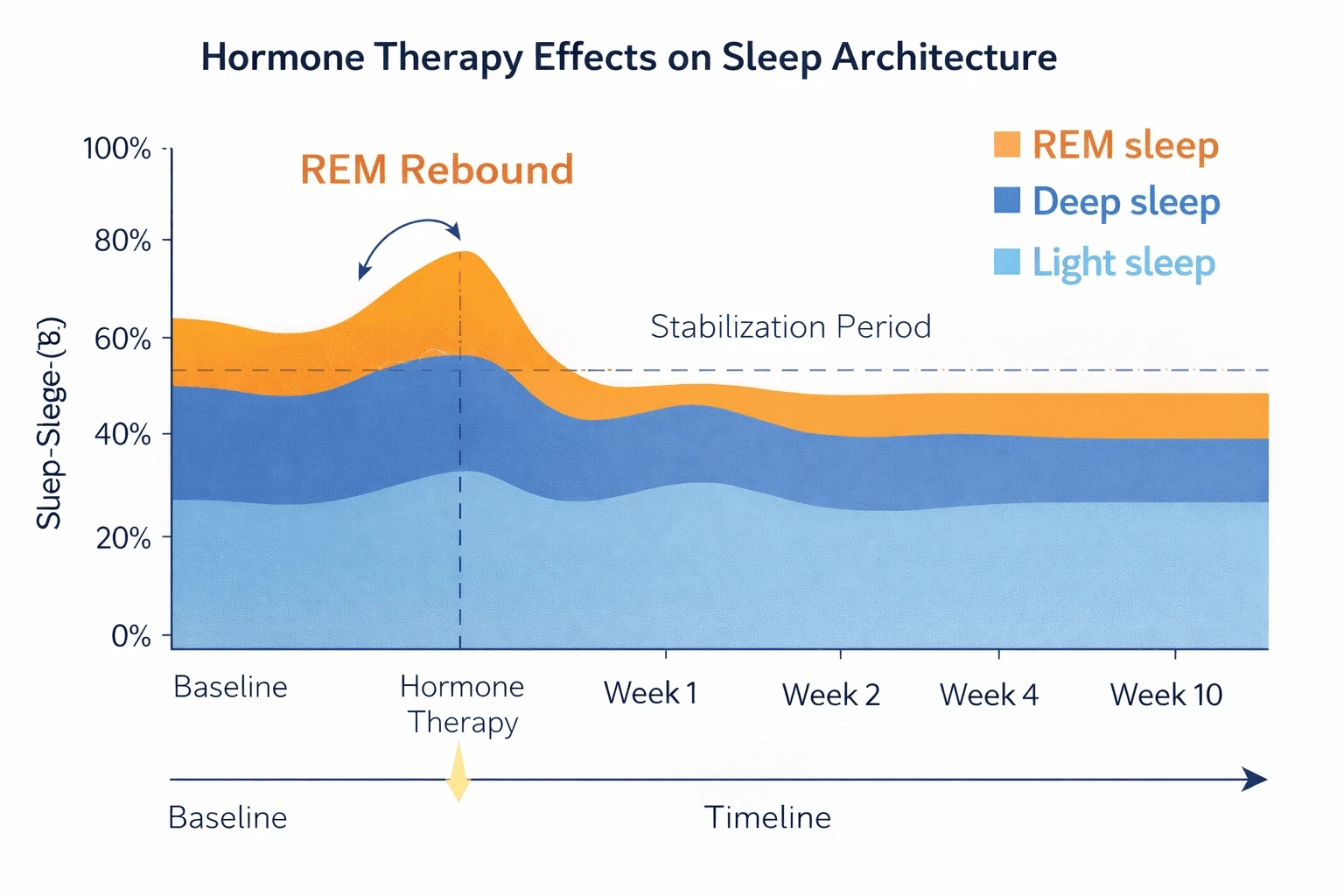
A small subset of women experience nightmare intensification when starting HT, typically in weeks 2-4. This represents a REM rebound phenomenon—chronic sleep deprivation has suppressed REM sleep, and as sleep architecture normalizes, the brain temporarily over-compensates with increased REM density and dream activity.
This worsening is actually a positive sign indicating treatment is working, though it feels counterintuitive. Nightmares typically peak around week 3-4, then decline sharply by week 6-8. Adding temporary low-dose trazodone (25-50mg) during this transition period can ease the REM rebound without long-term dependency.
The critical mistake: discontinuing HT during this window, assuming it's "not working" or "making things worse." Persist through this temporary phase—the neurochemical recalibration requires patience.
The Trade-Off Between REM Suppression and Dream Quality
Many sleep medications—particularly benzodiazepines, Z-drugs, and tricyclic antidepressants—reduce nightmare frequency by suppressing REM sleep entirely. This creates a false resolution: you stop having disturbing dreams because you stop dreaming meaningfully at all.
The cost becomes apparent over months: REM sleep consolidates emotional memories and supports cognitive function. Women who suppress REM chronically report feeling emotionally "flat," struggle with memory consolidation, and paradoxically report daytime anxiety that wasn't present before medication. You've traded nightmare distress for subtle cognitive and emotional blunting.
The honest limitation: Some women, particularly those unable to use HT, must choose between nightmare distress and REM suppression with its attendant costs. Neither option is ideal. This represents a genuine treatment dilemma where doctors should present the trade-offs explicitly rather than positioning sleep medications as pure solutions.
If you choose REM-suppressing medication for quality of life, use the minimum effective dose and attempt periodic tapers. Some women find they can transition off once through the worst perimenopausal volatility, even without HT.
The experience of nightmares and perimenopause together represents one of menopause transition's most underappreciated burdens. Unlike hot flashes visible to others, nightmare suffering remains private—yet it profoundly impacts quality of life, relationships, and daytime functioning. Effective management requires recognizing this as a primary neurobiological symptom deserving direct treatment, not a psychological problem requiring you to "cope better." For women who respond to hormone therapy, nightmares typically resolve substantially. For those unable to use HT, the path involves accepting some limitations while optimizing available alternatives—an honest assessment that respects both evidence and lived experience.