Understanding Skin Changes During Menopause
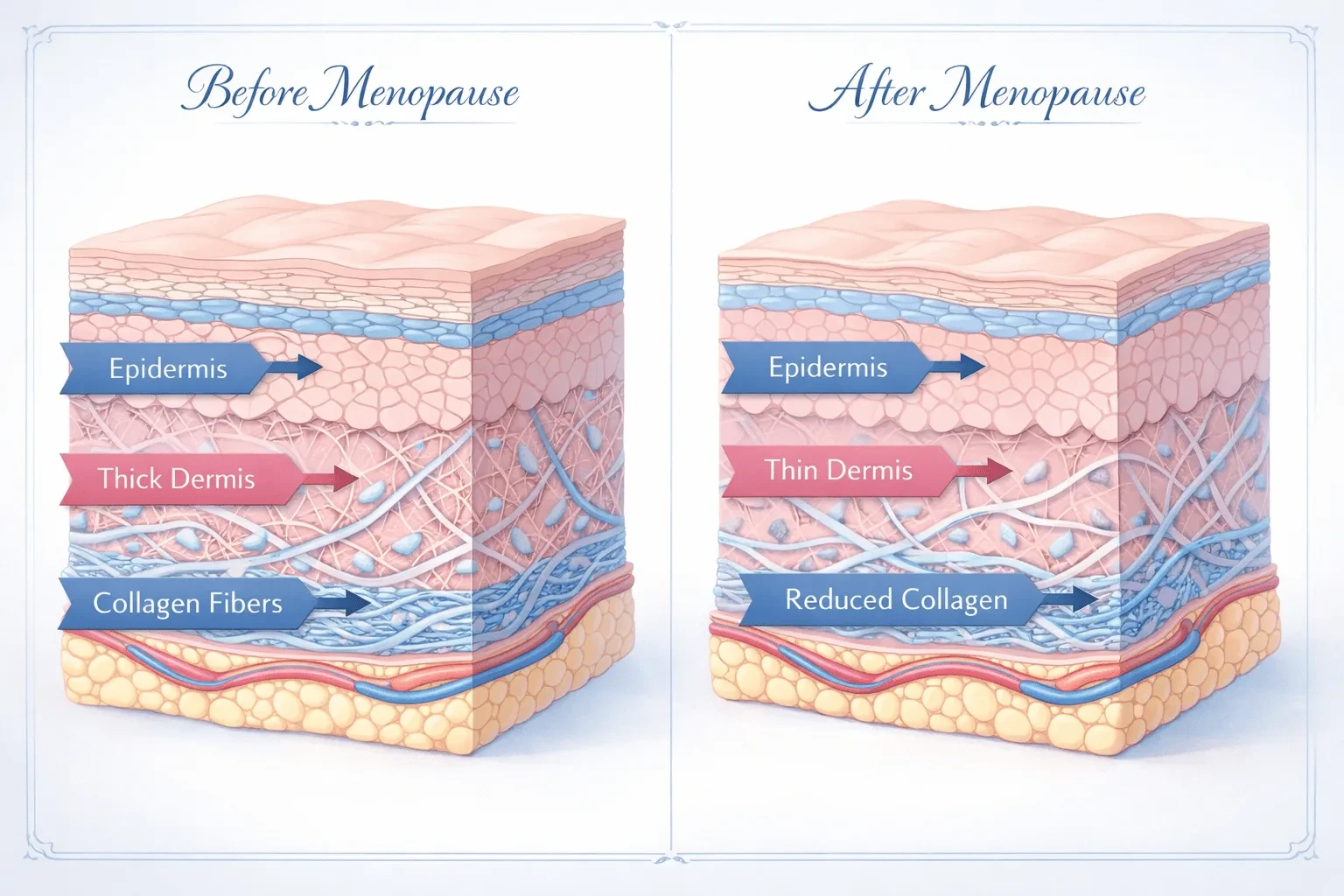
During menopause, declining estrogen levels trigger profound changes in skin structure that standard moisturizers cannot address. Estrogen receptors in the skin regulate collagen production, sebum secretion, and barrier function. When estrogen drops by up to 60% during perimenopause, skin loses approximately 30% of its collagen in the first five years after menopause begins. This isn't just dryness—it's a fundamental restructuring of dermal architecture.
The cascade includes reduced hyaluronic acid synthesis, compromised lipid barrier, decreased elastin fibers, and slower cell turnover. Women report that previously effective products suddenly stop working because the skin's needs have fundamentally shifted. A menopause face cream must address these specific hormonal changes rather than simply providing surface hydration.
Three distinct phases characterize menopausal skin changes. Early perimenopause brings increased sensitivity and unpredictable oiliness or dryness as hormones fluctuate wildly. Mid-transition shows accelerated collagen loss and pronounced fine lines around the eyes and mouth. Post-menopause stabilizes hormonally but requires ongoing support to maintain skin density and resilience. Understanding your current phase determines which skincare for menopausal skin formulations will deliver results.
The connection between skin changes and systemic hormonal shifts means that topical treatments work synergistically with other interventions. Women using hormone replacement therapy often report better results from skincare products because the skin retains more receptor activity. However, topical solutions remain effective even without HRT when formulated with the right active ingredients.
Common Myths vs. What Actually Works
Myth: Heavier Creams Are Better for Menopausal Skin
Many women switch to thick, occlusive creams when skin feels dry, but this often backfires. Menopausal skin needs functional ingredients that penetrate, not just surface occlusives. Heavy creams can trap inactive ingredients on the surface while blocking active delivery. Clinical studies show that lightweight serums with peptides, retinoids, and growth factors layered under a moderate moisturizer outperform single heavy creams by significant margins.
The texture preference depends on your environment and individual oil production. Women in humid climates often find gel-creams more effective than traditional balms. The key is active ingredient concentration, not weight or richness. A well-formulated lightweight cream with 5% niacinamide and peptides delivers better results than a petroleum-heavy ointment with minimal actives.
Myth: Retinol Is Too Harsh for Menopausal Skin
This widespread belief causes women to avoid the single most evidence-backed ingredient for collagen synthesis. The truth is more nuanced: menopausal skin often tolerates retinoids poorly at first because barrier function is compromised, but properly introduced retinoids remain the gold standard for addressing structural aging. Research demonstrates that low-dose retinol (0.25-0.5%) used twice weekly and gradually increased produces collagen benefits without the inflammation that triggers sensitivity.
The strategy involves barrier repair first, retinoid introduction second. Spend 4-6 weeks strengthening the skin barrier with ceramides and cholesterol-rich formulations before introducing retinoids. Many women who previously failed with retinol succeed when they repair the foundation first. Combining retinoids with strategic vitamin C application enhances collagen production while minimizing irritation.
Myth: Natural Ingredients Are Safer During Menopause
Plant-based skincare appeals to women seeking gentler options, but botanical ingredients can be more sensitizing than synthetic actives. Essential oils, plant extracts, and natural fragrances frequently trigger contact dermatitis in hormonally shifting skin. The contradiction here is striking: synthetic peptides, lab-created hyaluronic acid, and pharmaceutical-grade niacinamide typically cause fewer reactions than complex plant formulations with dozens of compounds.
Evidence-based menopause skincare brands increasingly use biomimetic ingredients—lab-created versions of compounds the skin naturally produces. These include synthetic ceramides that match skin lipids exactly, lab-grown growth factors, and precisely dosed peptides. The purity and consistency of synthetic actives often deliver superior results with lower sensitization risk compared to variable plant extracts.

Practical Strategies That Work
The Three-Layer Approach for Maximum Efficacy
Experienced practitioners structure skincare for menopausal skin in three distinct functional layers rather than applying a single multi-purpose cream. The treatment layer delivers active ingredients that stimulate cellular activity—retinoids, peptides, growth factors, or antioxidants. The hydration layer replenishes water-binding molecules with hyaluronic acid, glycerin, or polyglutamic acid. The barrier layer seals everything with ceramides, cholesterol, and fatty acids that mimic skin's natural lipid matrix.
This staged approach allows each ingredient category to function optimally. Apply treatments to clean skin when receptors are most available. Layer hydrators while skin is still slightly damp to enhance penetration. Seal with barrier protection to prevent trans-epidermal water loss. Women who previously found menopause face cream insufficient often succeed with this systematic layering because each product performs its specific function without compromise.
Evidence-Based Ingredient Combinations
Clinical trials consistently identify specific ingredient pairings that synergize for menopausal skin. The combination of niacinamide (5%) with peptides improves barrier function while stimulating collagen better than either alone. Retinoids paired with antioxidants reduce irritation while enhancing efficacy. Hyaluronic acid works more effectively when combined with occlusives that prevent its moisture from evaporating.
- Morning protocol: Antioxidants (vitamin C or E), hydrating serum with hyaluronic acid, broad-spectrum SPF 50. UV damage accelerates collagen loss exponentially during menopause.
- Evening protocol: Retinoid or peptide treatment, barrier-repair moisturizer with ceramides. Skin repair peaks during sleep when cortisol is lowest.
- Weekly intensive: Chemical exfoliant (lactic or mandelic acid) followed by nourishing mask. Exfoliation becomes more critical as cell turnover slows.
The timing matters as much as the products. Many women apply their entire routine immediately after cleansing, but strategic pausing enhances results. Allow 2-3 minutes between treatment serums and moisturizers for active ingredient penetration. Learn how vitamin C and hyaluronic acid work together to maximize hydration and antioxidant protection simultaneously.
Adjusting for Different Menopausal Phases
Beginners often misunderstand that skincare needs shift throughout menopausal transition. Early perimenopause with hormonal fluctuations requires flexibility—products that worked yesterday may irritate today. Keep a simplified routine with gentle, adaptable formulations. Mid-transition allows more aggressive intervention as hormones stabilize at lower levels. This is when retinoids, peptides, and growth factors deliver maximum impact.
Post-menopause shifts focus from correction to maintenance. Women five years past menopause report that consistent daily care matters more than intensive treatments. The skin has adapted to its new hormonal reality, and gentle, sustained support preserves results better than periodic aggressive interventions. This phase also shows the clearest benefits from in-office treatments like micro-needling or laser, which topicals then help maintain.

When Standard Advice Fails
The Surgical Menopause Exception
Women who undergo surgical menopause through oophorectomy face dramatically different skin challenges than those transitioning naturally. The abrupt, complete cessation of estrogen causes skin changes to accelerate at three to five times the normal rate. Standard skin cream for menopause recommendations prove inadequate because the timeline compresses years of change into months.
These women typically require prescription-strength interventions much earlier. Topical estrogen creams prescribed by dermatologists deliver hormones directly to skin without systemic absorption. Tretinoin at higher concentrations (0.1%) may be necessary rather than over-the-counter retinol. The layering approach remains valid, but active ingredient percentages need increasing to 2-3 times normal recommendations. Professional treatments become essential rather than optional—what naturally menopausal women might achieve with home care alone requires clinical intervention for surgical menopause patients.
When Skin Becomes More Oily, Not Dry
Approximately 15-20% of menopausal women experience increased oiliness rather than the expected dryness. This counterintuitive response occurs when androgens become proportionally dominant as estrogen declines, stimulating sebaceous glands. Standard menopausal skincare emphasizes rich, emollient formulations that exacerbate this condition, causing breakouts and congestion.
The solution inverts conventional wisdom: these women need lightweight, mattifying menopause face cream options with niacinamide to regulate sebum production, salicylic acid to prevent congestion, and water-based rather than oil-based hydration. They still need collagen-supporting actives like retinoids and peptides, but delivered in gel or lotion formulations rather than traditional creams. This subset often benefits from consulting both a dermatologist and endocrinologist to address the underlying hormonal pattern.
The Concurrent Autoimmune Challenge
Women with autoimmune conditions like lupus, rosacea, or eczema face compounding challenges during menopause. Hormonal changes can trigger autoimmune flares while simultaneously demanding more aggressive skincare intervention. The trade-off becomes apparent: ingredients that address collagen loss may trigger inflammatory responses in compromised skin.
Success requires prioritizing barrier protection and anti-inflammatory support over aggressive anti-aging actives. Instead of retinoids, these women often fare better with bakuchiol—a plant-derived retinol alternative with similar collagen benefits but minimal irritation. Peptides must be carefully selected for low sensitization profiles. Growth factors derived from plant sources rather than animal sources reduce allergic risk. The emphasis shifts from maximum efficacy to sustainable tolerance, accepting slightly slower results in exchange for avoiding setbacks from inflammatory flares.
Medical supervision becomes essential for this population. Many dermatologists recommend alternating intensive treatment weeks with recovery weeks, using prescription anti-inflammatories to control autoimmune activity before resuming collagen-building protocols. The limitation of standard advice is assuming everyone can tolerate continuous active ingredient use—autoimmune patients require cyclical approaches that honor their immune system's variability.